Addressing Systemic Racism in Action: Understanding the Mental Health Professionals’ Tools for Change
Addressing Systemic Racism in Action: Understanding the Mental Health Professionals’ Tools for Change
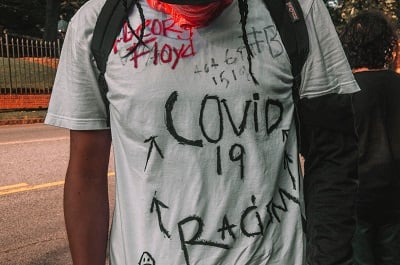
In the midst of the ongoing COVID-19 pandemic, the killings of George Floyd, Ahmaud Arbery, Breonna Taylor, and many others shine a glaring light on the continued presence of systemic racism in the police system and many other U.S. institutions. Despite calls for change within the Black community and among allies, little change has occurred over decades, as our laws and policies continue to promote systematic white privilege.
Although Black individuals account for only 13% of the U.S. population, they are being killed by police at more than twice the rate of White individuals in the U.S. Experts suggest that continued racism-related chronic stress remains high among this population and the evidence of detrimental impacts on physical (e.g., cortisol levels) and mental health (e.g., anxiety, depression) due to experiencing this chronic stressor is overwhelming (Pascoe & Smart Richman, 2009; Carter et al., 2019).
Psychiatrists, psychologists, and other mental health professionals are challenged to effectively respond to the mental health needs of communities of color. There are few Black psychiatrists and psychologists, there is a justified history of mistrust in the Black community towards the medical profession, and there is minimal training for white providers that addresses experiencing racism and its myriad consequences. Many providers feel ill-equipped to discuss systemic racism and the negative impact on health in the context of treatment. Nonetheless, Black clients need skilled therapeutic interventions to promote optimal functioning. To enhance the likelihood of effective treatment we present several solution focused tools for mental health professionals who have the privilege, power, and/or desire to make a positive impact in this crucial time.
Educate yourself
It is critical that providers seek to educate themselves on what systemic racism is and how it impacts all aspects of the current system and our clients of color. There are numerous resources available to provide historical context and emphasize white privilege and white fragility, and the meaning of anti-racism.
This education is vital and must come before providers can effectively provide emotional support without further invalidating Black clients’ reaction to the recent deaths and other daily injustices. Become familiar with facts about George Floyd, Ahmaud Arbery, and Breonna Taylor in preparation for discussing how these deaths are impacting our clients personally. It is vital that we not only allow but encourage our clients to discuss their emotions related to systemic racism; avoiding such discussions sends the message that the emotional toll of systemic racism is not worthy of discussion in the context of treatment.
Active Listening and Reflecting
When engaging a client in a discussion about how systemic racism impacts their personal well-being, it is imperative that we actively listen to our Black clients during these discussions and avoid acting based on feelings of defense, anxiety, and/or guilt. It is important for clinicians to be mindful that effective science-driven techniques based on cognitive behavioral therapy (CBT) such as cognitive restructuring can be invalidating to patients of color. Experts in addressing race-based stress underscore the importance of emotionally processing the deadly nature of systemic racism and warn against utilizing restructuring skills early on in this process (Carlson et al., 2018). Further, utilizing reflective listening skills during this discussion can help to increase engagement in the conversation [for more information about using reflective listening, see Miller and Rollnick (2002) and Bennett-Levy (2006)] By focusing on empathetic listening, we can further understand how systemic racism impacts our clients’ clinical presentations.
Staying Connected
Finally, encouraging Black and Brown clients to connect with their community for support is vital now more than ever. The COVID-19 pandemic has likely increased isolation; as providers, we can encourage Black clients to reach out virtually to valued community/religious organizations, meditation services, or other valued behaviors based in their community to help support them during this period of stress and uncertainty. Often, clients may have a desire to join with others but may have barriers that impact their ability to connect. By encouraging clients to actively identify and problem solve any such barriers (e.g., lack of knowledge about community services, lack of desire to engage), providers can help support individuals’ self-efficacy.
This is a time of continuing education for the mental health workforce to prepare for a potential increase in Black and Brown clients who are interested in clinical services due to the impact of systemic racism. By being proactive, we can make an enormous impact on the ramifications of racism and our actions can serve as an experiential example of repairing the relationship between communities of color and professionals in positions of authority.













