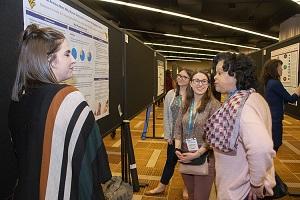
GET INVOLVED
Learn. Share. Network.

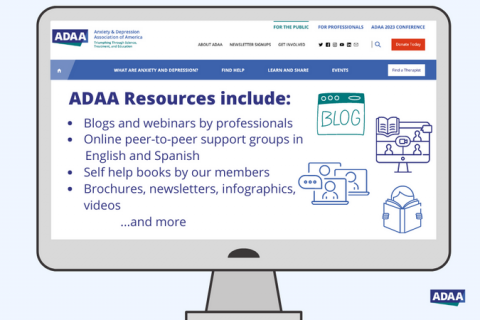
FREE Mental Health Resources for Your Clients/Patients
ADAA's website offers free expert reviewed content to supplement your client and patient's treatment. Clinicians, discover the additional resources including webinars, blogs posts, and more to share with your clients/patients.
Learn More

Career Center, Job Board & Professional Development
ADAA Mental Health Career Center - Share Your Job Openings. Post your Resume & Find a Job.
Learn More
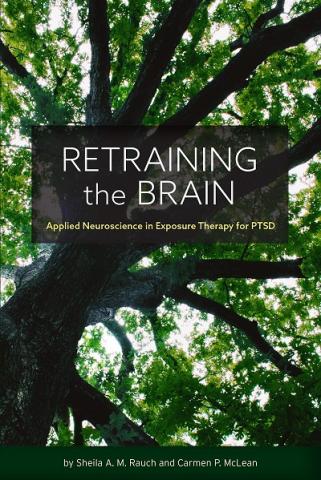
ADAA Journal of Mood & Anxiety Disorders TM
Submit Today! Read the current issue of ADAA's official open access online Journal of Mood & Anxiety Disorders TM.
Learn More