What Happened to My Child? Understanding and Treating “Bad Thought” OCD in Children
What Happened to My Child? Understanding and Treating “Bad Thought” OCD in Children

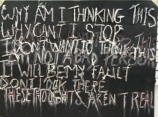
What is a parent to do? What is a parent to think when out of the blue their child comes to tell you I think I touched your private parts, I just made a deal with the devil, or most scary, I think I want to kill myself? Many people know something about OCD, they might think about handwashing, checking, or counting, but there is another aspect of OCD that is not often talked about or even understood by the public. For lack of a more technical term, let's call it bad thought OCD- intrusive thoughts of harm to self or others, inappropriate sexual thoughts, thoughts about God or religion, or simply doubt about one's actions.
Red flags for bad thought OCD
- Your gentle child talks about thoughts of violently hurting others even his family
- Your faithful child talks about hating God or making deals with the Devil
- Your easily embarrassed child describes thoughts of unusual sex acts
- Your well-behaved child thinks they lied, swore or cheated
- Your cautious child drank poison or swallowed something
- Your kind child begins to review every small not nice act he did in their life
One of the hardest parts is children feel that the upsetting thoughts are coming from them or are their own thoughts. Maybe they really feel or want to do what their brain is telling or secretly want to feel that way. Kids can keep these thoughts to themselves (especially adolescents). Children or teens can become grumpy and irritable or avoid things they need or want to do.
How to know it's OCD
If possible, get a thorough assessment with a therapist familiar with childhood OCD.
Parents and children will notice that in contrast to their usual thoughts:
- The thoughts barge in out of the blue (for example - playing with friend and think wants to stab them, feeling happy and think suicide)
- Content of thoughts contrary to child's general personality
- The child is very distressed about thoughts and tries to avoid them
- The child may do rituals repeatedly when has the thought (confessing, praying, apologizing)
Bad thought OCD is TREATABLE
A number of the techniques therapists use for other forms of OCD are helpful with these OCD symptoms as well. There are a few modifications that are specific to this form of OCD. The first thing is EDUCATING the child and family about what is happening in the child's brain. Their brain is misfiring or hiccupping, sending out a nonsense message wrapped in very scary packaging. The child needs to know that it is his reaction to the thought that is causing the problem- the thought is scaring them because they think it is important and has to mean something.
Therapists teach kids to:
- Let the thought come in and go out like any other thought- don't try to stop it, don't push the pause button, don't try and force it out, play out the movie
- Relabel- It's not me - it's OCD, I am not weird - OCD is weird
- No thought, no matter how horrible, changes the person I am
- Just because I have the thought, doesn't mean I want to do it
- Break OCD rules - don't do or do the opposite of what it says
Identifying rituals and avoidance
The most common rituals for this form of OCD is confessing thoughts to parents and seeking reassurance. While this is the most distressing part for parents, the good news is that if the parents are involved, they can help their children. Therapists work with children and their families to reduce rituals step by step - using tell times or coupons to trade in for thoughts.
Mental rituals are harder to identify but therapists familiar with OCD know how to ask. Some examples include:
- Does the child think of a positive word or create a good picture is his head to neutralize the bad image?
- Does the child say a prayer, a special word, or does he think to himself I am a good person?
- Does the child mentally review his day in his head to make sure he did not do something bad?
The therapists work with children to change and eliminate these mental rituals through:
- Avoidance- not touching or looking at knives or scissors, not going to church, concern about poisons. With all forms of OCD we have to eliminate avoidance and approach what you fear.
- Imaginal exposure - we have children play with the words or images they avoid, say it in a funny voice or sing it (like harm or kill). For older children and teens we have them write out the story that OCD is scaring them with and record and listen or read it over and over again. It wears out the fear tape.
Summary
The good news is although this is scary stuff - this form of OCD is very treatable. Often this can be done with exposure and response prevention (ERP) alone. However, sometimes a child is just too depressed, too overwhelmed, or too bombarded by thoughts to do the treatment or function in their life. Medication can be helpful in turning down the volume and distress of these intrusive thoughts and making it more possible to address the rituals.
The therapist will design the treatment plan for your child, but the parents' role is also important because children look to their parents for their reactions as well as their support. The parents' job is to be brave too, and to show their child that they are not afraid of their child's fears.