ADAA Mental Health Blogs
ADAA's evidence-based mental health blog featuring mental health professionals.
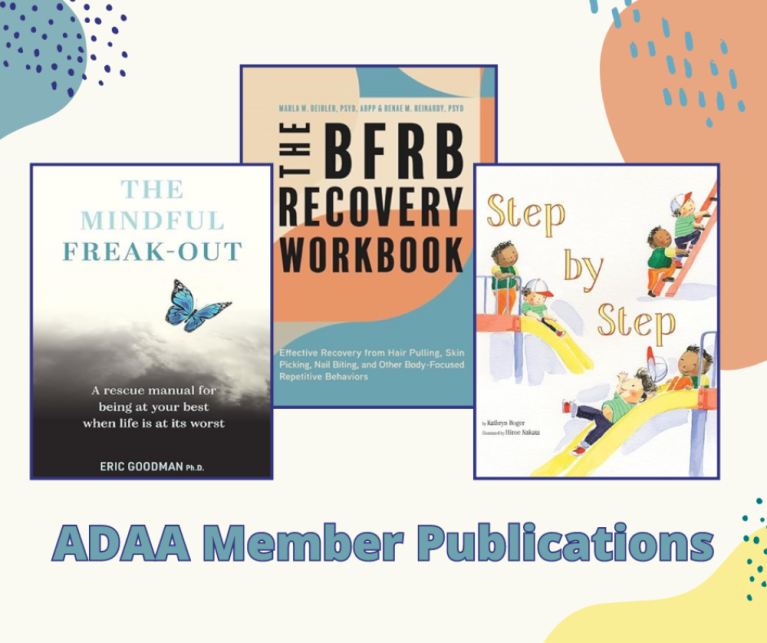
Every quarter ADAA interviews three members for a blog that showcases new books by our esteemed experts. Our series – “In Conversation With ADAA Member Authors” – is a wonderful way to highlight our members' expertise and provide not only a brief synopsis of their books' focus areas but gives members a chance to relay in their own words what’s special or important about their respective publication(s).
Suicide rates in teens have been steadily on the rise over the past two decades, and data from the 2021 CDC Youth Risk Behavior Survey found that approximately 22% of teens reported suicidal thoughts and 10% of teens reported doing something to try to end their life in the past 12 months. Given that many teens are experiencing suicidal thoughts, it is important for parents and caregivers to know how to talk to their child about their mental health.
Ask Your Child Directly
While treatment for OCD is highly effective for many, it can be hard work! It’s not an uncommon experience to lose momentum midway through treatment or even in the final stages. Below are some helpful tips from an OCD specialist to help you make it across the finish line!
1. Watch out for assigning the hard work to your “Future Self”
City life is attractive to many people, but seemingly endless high-rises and gridlocked traffic leave little room for city dwellers to reap the benefits that green spaces may have to offer. In our rapidly urbanizing world, more than half of the global population have made their homes in cities. Unfortunately, as we migrate to urban areas, access to green spaces is dropping, which may actually affect our mental well-being.
Individuals residing in cities are:
It’s common for a new mother to experience thoughts or worries about her newborn child. I remember the worrying thoughts I had shortly after my son was born when I left for an ADAA conference for a few days. A call from the nanny saying he was sick cut short my trip and I was on the first plane back home. I worried the entire flight. I ruminated about him being sick; I was anxious and I scolded myself for leaving him. But when I saw him and realized that he would be fine, my anxiety subsided.
Cognitive Behavioral Therapy for Tinnitus: Reduce Distress, Improve Functioning, Promote Habituation
In true form, for OCD lovers like myself, I posed more questions than answers in the title. That was intentional, to be funny, eye-catching, and thought-provoking. Hopefully, I pulled off at least two of those. These questions are often asked by clinicians, and sufferers alike. How do I know if this is OCD or if this is social anxiety? I’ll focus on answering this question as best as I can.
Getting a good night’s sleep provides many benefits. It reduces stress, supports health satisfaction, and allows one to feel overall more balanced. What happens though if the bed becomes associated with repeated stress, anxiety, and constant sleepless nights? This is the life of someone struggling with chronic insomnia.
This blog was originally posted on Ten Percent Happier on April 22, 2022 and is reprinted here with permission
I grew up in Brazil, in a little town called Governador Valadares. Early on, my father left us, and it was my mom, my sister and me. Things were challenging. My mom did the best she could, she worked as hard as she could. But I remember how tough things were – there were times when we didn’t have enough to eat. But we kept going.
The Russian invasion of Ukraine is a bitter reminder that there is no end to the horrific suffering that humans are sometimes willing to inflict on others.
Many members of BIPOC communities deal with stress and trauma that can stem from specific socioeconomic struggles that consciously and subconsciously impact the everyday lives of the community.
In a world that is constantly evolving, BIPOC youth are actively working to change the way their communities acknowledge and embrace mental health. Youth (defined here as those between the ages of 15 to 24) are redefining what mental health means and are trying to “unlearn” some of the negative stigmas that have been taught or demonstrated by older generations.
“Polina came to our bedroom awakened by the sound of explosions. I didn’t know and still don’t know what to tell her. Her eyes today are full of fear and terror; eyes of all of us.”
Alina, a family friend who is a marketer and mother of two children from the Ukrainian capital of Kyiv – which is under seige by Russian forces – shared this reflection on her Instagram story. Her daughter Polina is 7 years old.
Self-Compassion: The Art of Tending to Your Struggles with Loving-kindness Instead of Self-criticism
Another school year has come around and with it, the possibility of extreme fear and separation anxiety for some children. Although it’s normal for any kid to have a certain degree of back to school anxiety, there is a huge difference between a child who is nervous about the new school year and one whose anxiety is severe enough to seek professional care.
As the school year begins, children who normally go through separation anxiety may be even more anxious about going back into the classroom during the pandemic. After all, the beginning of a new school year can be threatening during normal times, but returning into a situation where the coronavirus is likely to be present has raised anxiety levels in many kids and parents.
If you find that you’re not sleeping enough—you’re not alone. According to the Center for Disease Control (CDC), about 35% of American adults skimp on sleep; and this rate is even higher in African Americans and other minority groups. This is an important public health concern because getting a good night’s rest is essential for physical and mental wellbeing.
My friend’s phone call left me stunned and shaken. She had just been released from the hospital, where she had been admitted for suicidal ideation. “Suicidal ideation” was an unfamiliar term to me, but I could easily figure what it meant. Carolyn had been grieving a loss, but I had no idea that she had become depressed and suicidal. For me, Carolyn, and her family, it was the beginning of a long journey in coming to understand depression and so many of the other conditions that ride at its side.
April is world autism awareness month, and so there is no better time to bring to light not only the challenges associated with autism, but also the most common conditions that impact this community. Children and adults on the autism spectrum are more likely to have an anxiety disorder than others. And research suggests they also may face challenges with getting an anxiety diagnosis and treatment.
One year ago, the world tuned in to see a man being murdered by a uniformed police officer while onlookers pleaded for mercy. George Floyd’s death led to numerous protests all over the world against police brutality and systemic racism experienced by Black and Brown communities. Although conviction in cases involving police killings are rare, many hoped that the outcome of this trial will be different. Perhaps the video and the parade of witnesses and experts will be enough this time.
It can be challenging to know when to seek therapy and how to get connected with care. Talking to your primary care provider is one option.
Primary care plays an important role in helping us to be healthy. You may visit your primary care provider when you feel sick, if you develop a new symptom, or once a year for an annual wellness visit. Primary care providers can also help if you are concerned about your mental health.
Anxiety is one of the most common mental health disorders affecting those on the autism spectrum. Anxiety can cause extreme fear, dread, sweating, restlessness, and even chest pain. “A lot of us do experience anxiety, and we struggle with it in our own ways,” says Jairo E. Arana, an autistic member of the Community Advisory Council for SPARK, the largest study of autism.
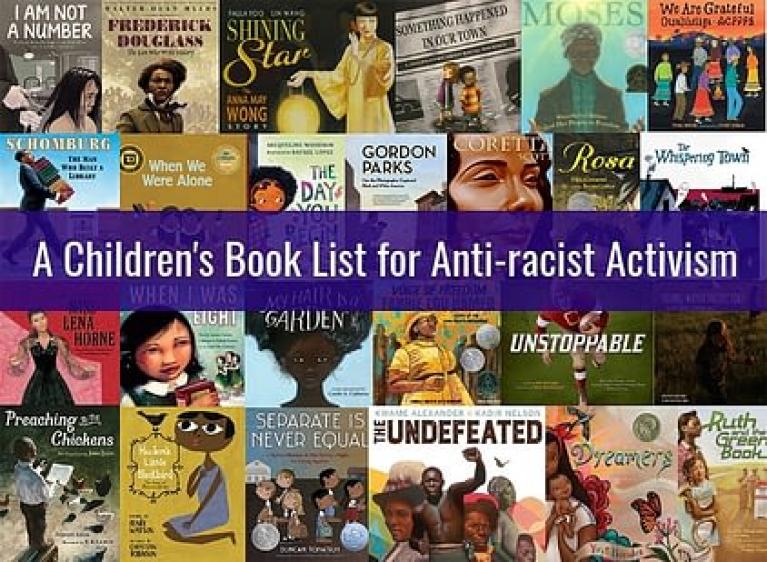
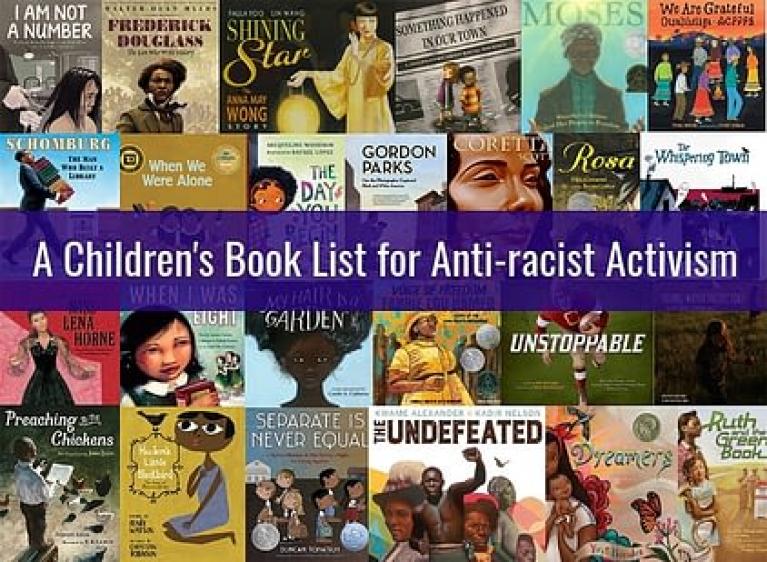
Parenting is an increasingly complex job. It’s layered with important responsibilities one of which is raising anti-racist children. In addition to being a Registered Psychologist, I am also a parent, a white parent, who wonders what I can do to engage with this important work. I have learned that I can be doing more at home to raise antiracist children, and that the responsibility is mine and not that of the Black and Brown communities.
The deadly shootings of eight people in Atlanta on March 16 and 10 people in Boulder, Colorado, on March 22 brought heartache and grief to the families and friends of the victims.
These events also take a toll on others, including those who witnessed the shooting, first responders, people who were nearby – and even those who heard about the shooting in the media.
I am a trauma and anxiety researcher and clinician, and I know that the effects of such violence reach millions. While the immediate survivors are most affected, the rest of society suffers, too.
As with many other physicians, recommending physical activity to patients was just a doctor chore for me – until a few years ago. That was because I myself was not very active. Over the years, as I picked up boxing and became more active, I got firsthand experience of positive impacts on my mind. I also started researching the effects of dance and movement therapies on trauma and anxiety in refugee children, and I learned a lot more about the neurobiology of exercise.
The news of the world can be scary for children and teens (and adults for that matter). Whether it’s rioting in the U.S. Capitol, looting in the streets of Portland, or people dying of COVID in the hospitals of New York, images of out-of-control behavior and death can be terrifying. When my son was a young teenager, he loved to watch horror movies but dashed out of the room at the first sight of the nightly news. He understood that it was real and it scared him because he imagined that someone else’s reality could extend into his world.
Symptoms of depression, anxiety and obsessive compulsive disorders have emerged or worsened for many during the pandemic. This is no surprise to clinicians and scientists, who have been increasing worldwide access to mental health information and resources.
I recently had a Zoom call with a patient who leaves deliveries on her porch for a week and then disinfects the packages before opening them. Another patient shared how upon returning home she removes all her clothes in the garage, sprays her body with rubbing alcohol, and immediately showers. Following those two sessions, I walked outside and saw a man driving alone in his car wearing a mask. A female jogger, across the street, was wearing a mask too. She was by herself, a hundred yards from the nearest person.
About a year ago I began to follow my interest in health and fitness on Instagram. Soon I began to see more and more fitness-related accounts, groups, posts and ads. I kept clicking and following, and eventually my Instagram became all about fit people, fitness and motivational material, and advertisements. Does this sound familiar?
1. How can you know if something is an intrusive thought, or monkey brain, and what is a genuine desire to do something bad? Where do the intrusive thoughts even stem from?
2020 has been a difficult year for everyone, especially those who are prone to anxiety and depression. The social isolation, uncertainty about employment, income, health and the health of Covid vulnerable people you love has posed a unique challenge for us all. It is completely understandable for you to have some apprehension about the upcoming holidays.
In addition to its staggering impact on physical well-being and mortality, COVID-19 is also taking an unprecedented toll on our mental health. Numerous recent studies have shown global increases in the prevalence and severity of depression and anxiety as well as increases in post-traumatic stress disorder and substance abuse. These increases likely stem from the changes to daily life we have all been asked to make in attempts to mitigate viral spread.
The virus has upended the world as we know it, and kids are struggling. Kids were not meant to live this way. None of us were meant to live this way, but as a child therapist, I have a special focus on kids and their well-being.
During this time of national crisis, we must manage two things simultaneously: 1) Protect ourselves from the Coronavirus, and 2) Protect ourselves from anxiety. If your anxiety, fear, and worry has been overwhelming, put these ten strategies into practice.
“If we lose, I just don’t know whether the country can survive,” my client said. “Things are getting too crazy.” I heard those words before. From clients of the opposite party. The upcoming election has become every American’s—Republicans and Democrats, therapists and clients— worry number one. To many of us, the idea of losing feels like an existential threat, one that is igniting core fears about our health, our safety, our connections with our loved ones and community. We may be donating time and/or money to our campaign of choice, but it doesn’t feel like enough.
My OCD (obsessive-compulsive disorder) clients often ask me at some point early in therapy, "Why do I have OCD? Why is this happening to me?" While many environmental factors can play a role and a predisposition to OCD is certainly hereditary, the ultimate answer to this question is quite simple.
To answer it, we need to know what is different about people who develop OCD compared to people who do not develop OCD.
Steve has served as a police officer for 24 years, including being a SWAT team member for years. He and I have worked together on his traumatic experiences. He has told me that in a given day a police officer might have to deal with two to three overdoses and do CPR.
I was recently interviewed for an article on how the behaviors people use to avoid getting Covid 19 might make OCD worse or cause OCD to develop. After my interview the reporter notified me that the story was “killed” by the editor of the publication because he wanted to publish a story that suggested living through the pandemic would result in an increase in OCD or the development of OCD.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
If you engage in some positive distracting activities during this crisis, then the flow of the day will move like a steady stream rather than a slow drip.
Time might seem to go by slowly and you only measure your day by the time between newscasts.
Do not just stay glued to the tv related to the pandemic.
Look up a new recipe and try to cook it. Get creative with what you have in the pantry.
Let’s first acknowledge that going back-to-school is harder this year. As you write lesson plans, you’re trying to figure out how to execute them online. As you set up your classroom, you’re dodging the new partitions that have been installed. As you meet with your staff about the upcoming year, you struggle to regain a connection with them over Zoom or WebEx. You’re sitting through professional development that’s more about proper hygiene and about using personal protective equipment than curriculum development and teaching strategies.
My client Tom had been working from home since the pandemic hit in March, but now his boss had set a date for returning to the office, in only three weeks. Tom felt anxious about prolonged exposure to his co-workers, as his partner had an underlying health condition. He was stuck on what to do. Should he negotiate to continue working from home, or comply with his boss’s request to go back to the office? One choice could put his job at risk, the other his partner’s health.
Many parents around the country are being faced with deciding whether or not to have their children return to school — whether it be part-time or full-time — for the upcoming school year. For parents who suffer from significant anxiety, this can be a very difficult decision. The last thing any parent wants is to make a decision that won’t be in their child’s best interest, or that causes the child to be exposed to the coronavirus.
The COVID-19 pandemic has rapidly and abruptly changed human life in unexpected ways. In the last few months, since the COVID-19 stay at home restrictions came into place, millions of people have been working from home and practicing social distancing. As the lockdown restrictions are getting lifted or eased in various places, most people are experiencing some degree of re-entry anxiety, as they contemplate or attempt to navigate some degree of resumption of required pre-lockdown activities, such as going to work.
Today I said thank you to the staff at the senior living facility where my 97-year-old grandmother lives. At the outbreak of COVID-19, she found herself hospitalized with bacterial pneumonia – nothing related to COVID-19. Just poor timing.
Racial and related inequities have immensely traumatized Black and Brown citizens of the United States for centuries. The COVID-19 pandemic and its rates of infection, disease burden, and fatality have unprecedentedly exposed the devastating consequences of racially defined health, mortality, and economic disparities in the US.
Images of the murder of Black Americans, discussions about systemic racism, sirens blaring, crowds protesting, curfews, fires. It’s tough for adults to make sense of the hurt in the world right now, but how do we help our children and teens with it?
Grief is a natural multifaceted reaction to loss.
We all have the capacity to adapt to even the most difficult loss.
Recognize that grief contains love; try to let it in and not push it away.
COVID brings new potential risk factors, such as physical distancing that can derail healing after loss.
In the grocery store, you are told to stand back on the red line. You feel ashamed for not seeing it in the first place.
You tell your in-laws you are not comfortable having them visit their grandchildren in person, and you worry that they may never forgive you.
Someone asks you to stand farther away from them, and you feel embarrassed for making them feel uncomfortable.
Feeling anxious, worried, and tense? You are not alone! Anxiety disorders are the most common mental illness in the US, and General Anxiety Disorder (GAD) affects 6.8 million adults (or 3.1% of the population) every year (https://adaa.org/understanding-anxiety/facts-statistics). When feeling overwhelmed with worries and tension, the first step many people take is to ask their doctors about medication.
It is time to stop dreading anxiety.
Few things motivate escape and avoidance more than the feeling of anxiety, the sense of apprehension and worry that a catastrophic outcome may lie ahead. Sometimes we can name it – tomorrow is the big test, the first online date, a telemedicine check-up by Zoom – other times, we are unsure of the source of our unease. Of course, few words promote anxiety more than coronavirus.
The only thing certain in life is, seemingly, uncertainty. These days, especially, we don’t need to look very far to find uncertainty. We find it when we go to our local grocery store and see faces covered in masks, or when we turn on the news and hear that even our nation’s lead medical professionals don’t have the answers when it comes to stopping the COVID-19 pandemic.
There is a lot of anxiety surrounding the COVID-19 pandemic. Not only is there concern about getting sick, but financial strain, social isolation and uncertainty of the future are contributing to an increasingly concerned and nervous society. Many people have learned coping strategies to deal with anxiety, such as going to the gym, talking with friends and family, or attending peer support groups. Unfortunately, many of these supports have been eliminated or reduced due to social distancing requirements.
Unfortunately, there’s been no shortage of bad news lately – from COVID-19, to unemployment numbers, to businesses closing their doors. We’re living in unprecedented times, where many of us are stuck in our homes, and possibly fearful of the outside world and all that comes along with it. That certainly seems like an environment that would naturally breed anxiety, especially when it comes to finances.
The coronavirus has disrupted the schedules of Americans in ways not seen since -- well, maybe ever! Some of us have a lot more free time than before, and some have a lot more stress than before. Whichever of the two camps you’re in, mindfulness exercises have much to recommend them right now.
People deal with stress in different ways and while there is no right or wrong way to deal with the stress of a pandemic, I figured it would be helpful to share a few ways that I have found balance during this time.
Find Acceptance
For all athletes, the outbreak of COVID-19 brought competition to a striking halt. Many who were ramping up their training regimen for an upcoming tournament, or helping their team strengthen their playoff seeding, were heartbroken to hear there were no more games to be played. Some athletes have spoken publicly about their immense feelings of disappointment, sadness, and anger. However, some athletes who describe themselves as being more anxious in nature are reporting that the absence of competition has actually been more of a relief.
In this unprecedented novel coronavirus (COVID-19) pandemic, many parents are left struggling with navigating a new, uncharted territory of challenges, while trying to grapple with and establish new norms in the household. Given the rapid and drastic changes in daily life that the world has witnessed recently, it is not uncommon for parents to doubt their parenting approach, whether they are doing enough, and/or wonder about what else could they be doing. Many parents are understandably feeling overwhelmed.
Why Can’t I Stop Watching the News?
We are living with unprecedented levels of uncertainty right now. How long will the current restrictions last? When we will be able to see friends and family again? Will the economy recover? How do we keep ourselves and our loved ones safe?
Telling oneself not to be anxious during the COVID-19 pandemic is like trying to tell water not to be wet. These are anxious times. The question is not how can I be anxiety free right now, but how can I best manage the anxiety that shows up?
Life in the time of a pandemic is difficult. Our lives have suddenly and dramatically narrowed while we try to avoid an invisible threat which has been spreading across our planet. And where there is even the whiff of a threat, there is anxiety.
I’ve heard from friends countless times that they have considered therapy, but their lives were just too busy for it. Maybe when they had more time, they’d say.
What better a time than now, when you’re safe at home 24/7, and likely anxious about the world’s current state?
A cancer diagnosis brings a wealth of psychological challenges. In fact, adults living with cancer have a six-time higher risk for psychological disability than those not living with cancer. Patients and families have to deal with not only the physical stress to their lives and potential livelihoods, but also with family dynamics and changes in their sense of self and future.
If you are like most families with young children, these past few weeks have been filled with playing simple games, such as who can run the fastest from one side of the room to the other, or who can accurately recite the alphabet backwards. When my children were young, their favorite game involved my hiding their stuffed animals in the house.
Much of the mental health community is moving to teletherapy. While some parents and providers have experienced this type of therapy before, for many it’s brand new! Here are 10 teletherapy tips to help kids and teens get the most out of their teletherapy sessions:
1. Find a space.
You know that anxious feeling when you’re not sure what others think of you, leaving you with a sneaking suspicion that you’re making a fool of yourself? It’s called social anxiety. And while everyone has some social anxiety, for many, high social anxiety gets in the way of meaningful social connections and quality of life.
Experts suggest that the surge of COVID-19 patients is still coming for many hospitals in the United States and throughout the world. Health care workers on the frontline are waiting for a wave, a wave of unknown height and unknown force to hit the hospitals. In some areas that wave has already begun. Faced with harrowing tales from Italy and China, hospitals count supplies, teams shift staffing schedules, and providers fear the worst.
Yesterday I received an email from a former client with the subject line HELP!! Six months ago, Angie came to me with contamination OCD. Obsessed with germs, Angie washed her hands and used hand sanitizer compulsively, avoiding touching everything from the door handles to the magazines and armrests in the waiting room of my office. (Just like we all are now.) Working together, using incrementally progressive exposure response prevention, Angie’s obsessions and compulsions faded, and satisfied, she ended therapy.
Major crises raise people’s concern for personal safety and heighten anxiety. One effect of this heightened anxiety is that it can intensify bias and discrimination as we start focusing our attention on our own well-being. Throughout the COVID-19 crisis many individuals with disabilities and those managing medical conditions who face additional hurdles due to the alterations and disruptions to their lives have been reporting a lack of sensitivity towards their needs.
As many in the United States (US) stay home and practice social distancing to protect themselves from COVID-19, individuals from lower socioeconomic status (SES) backgrounds face heightened barriers and risks.
What if you have the kind of anxiety that makes you feel trapped and panicky because of the stay at home orders due to COVID-19? While there are some whose anxiety disorder might find it a relief to have to stay at home and engage in social distancing, there are many for whom this situation creates a special nightmare. This nightmare occurs for several understandable reasons. First, many people with panic disorder feel safer when they know they have easy access to emotional support and physical safety.
Coronavirus has turned our world upside down. Many businesses that typically require being present in person are shut down and unable to operate. Everyone is aware that in most places across the country right now, you can't do things like eat out at a restaurant or go to a nonessential doctor's appointment.
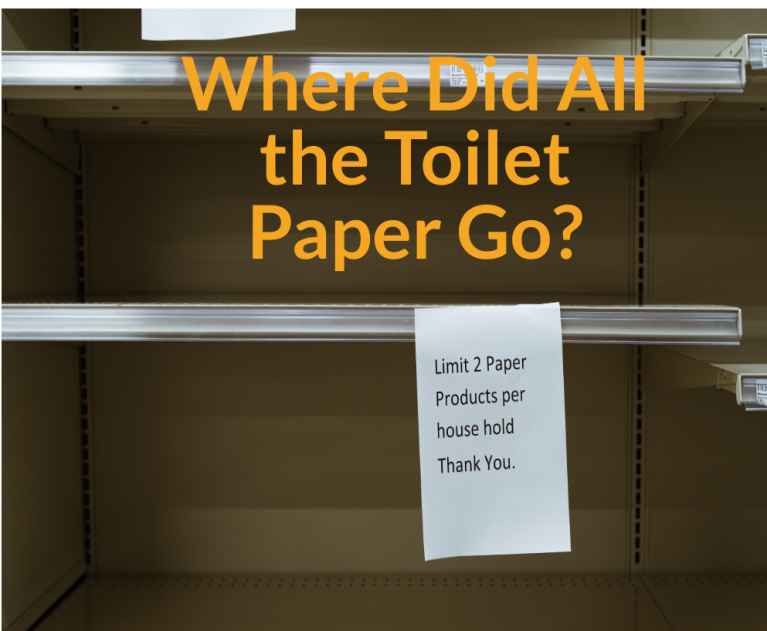
Hoarding behaviors range from the normal (i.e., acquiring and saving items we do not need and/or will not use) to the clinically diagnosable (i.e., having areas of your home that are not usable due to clutter). Most of us fall somewhere on this continuum. In times of crisis, humans and other animals can have an increased drive toward hoarding behaviors. However, these efforts to secure material resources can be problematic to the individual and our community.
Parents can't be constant companions, teachers or saints at this time. You can be enough.
Each of us is facing the challenges of the COVID-19 pandemic that impact our ability to respond effectively. Some of us are facing severe financial costs, heightened risk due to age or physical conditions, experiences of racism and other forms of discrimination, systemic inequities and injustices that make every adjustment more challenging and threatening, psychological challenges that heighten the impact of anxiety and isolation, jobs that require them to put themselves at risk, or the challenges of caring for ourselves and others alongside other demands.
Major crises raise people’s concern for personal safety and heighten anxiety. One effect of this heightened anxiety is that it can intensify bias and discrimination as we start focusing our attention on our own well-being.
What is Mindfulness?
Mindfulness is a term that is commonly used these days. What really is mindfulness?
Mindfulness involves bringing awareness to the present moment, through non-judgmental noticing and observing, with the goal of being fully present in the current moment.
Benefits of Mindfulness
I’m a specialist in the treatment of OCD and anxiety disorders. OCD is a debilitating mental health disorder whereby patients experience unwelcome, intrusive, disturbing thoughts (obsessions) that create anxiety.
Since the World Health Organization declared the COVID-19 outbreak a global pandemic, many of us, even those who have not been infected by the virus, will choose to quarantine in our homes for the upcoming weeks. Capsized travel plans, indefinite isolation, panic over scarce re-sources and information overload could be a recipe for unchecked anxiety and feelings of isolation. Here are a few pointers that could help you survive spiraling negative thoughts about this uncertain time.
1.) Reframe “I am stuck inside” to “I can finally focus on my home and myself”
Fear, uncertainty, and anxiety are bound to be heightened with wide-scale disease outbreaks that are contagious, particularly when they involve a new, previously unknown disease-causing agent, as is the case with the novel coronavirus (COVID-19) outbreak. This fear and anxiety can especially affect people already suffering from anxiety, and repeated news cycles about the spread of coronavirus do not help this anxiety.
Obsessive Compulsive Disorder (OCD) often wears down children and parents. Prior to beginning treatment, parents often state that they can no longer understand or recognize their child. They see their child as being rigid, stuck, and exhausting. They do not know how to respond to the grip OCD has on their child.
Family #1: Rachel avoids wearing clothes that make her feel itchy or uncomfortable. As a result, she insists on wearing the same outfit to school and at home. Rachel’s parents feel forced to wash her clothes daily to avoid conflict.
The onset of OCD typically occurs during adolescence, with 25% of cases starting by age 14. Because teens typically live at home, accommodations by family members are common. Accommodations occur when others attempt to aid sufferers by assisting in rituals.
Checking my email last night, I noticed that “coronavirus” appeared in the subject line of about 70% of the messages. It makes sense that the Wall Street Journal, CNN, Fox News, and The Washington Post would be featuring stories, but Wired and The Atlantic and other newsletters have all caught COVID-19 fever. The media are turning this into a payday. I don’t begrudge them that. Panic sells. It’s good business.
Are you feeling sad or lonely this Valentine’s Day? We don’t usually associate Valentine’s Day with depression, but if you’ve recently gone through a breakup or if you’re dealing with persistent disappointment in your love life, Valentine’s Day can be a depressing affair.
Emotions Related to Loss
Most of us started out playing sports for fun. Practices and games were a chance to meet up with friends (old and new), to get away from our work-a-day lives, and take on an athletic challenge that got our hearts pumping and our endorphins firing.
For many competitors, however, there’s a point at which the fun-dial gets turned down, and the pressure to perform makes our heads spin, our hands sweat, and we start fearing mistakes rather than embracing opportunities to improve.
Did you know the inability to experience your emotions causes anxious sensations? But that does not mean it's part of an anxiety condition.
One of my favorite concepts to challenge in session is the idea of "My Anxiety." It's often a term people will use when they are struggling with both an anxiety condition and emotional regulation. People suffering from an anxiety condition will often begin labeling uncomfortable emotions as an anxious state or part of an anxiety condition- like generalized anxiety, OCD, or panic disorder.
It’s easy to feel unsettled when we hear unsettling news on television or social media, particularly when several events happen at once. The combination of Kobe Bryant’s death, the fires in Australia, and the spread of the Corona virus, can trigger an escalation of anxiety or depression for those already in a fragile state. It’s normal to experience an emotional reaction to events such as these but we don’t want them to overwhelm us. We can prevent stories in the media from hitting us hard emotionally by taking four simple steps.
ADAA member Dave Carbonell, PhD wrote this blog post to accompany his new ADAA webinar.
“The harder I try, the worst it gets!”
Sometimes parents who seek consultation with me about their child’s worries or fears are surprised to learn that the child has Obsessive-Compulsive Disorder (OCD).
“But she doesn’t wash her hands all the time…”
Or they do not realize that certain symptoms are part of OCD.
“He had bad thoughts that bothered him. He used to tell us about all the time. To get away from that, he developed OCD and started worrying about germs.”
Let’s face it. The holidays can be stressful for anyone with all of the expectations for joy, gift giving and getting together with family, friends and co-workers. When you are prone to worry, social anxiety or depression, however, the pressure can feel doubled because you feel out of sync with all the expectations that apply pressure to your vulnerable spots. Here is some advice that could help you to feel better prepared to avoid the pitfalls of the holiday pressure to be something that you are not.
According to the National Highway Traffic Safety Administration, in 2016 alone, there were an estimated 7,277,000 police reported traffic accidents in the United States. Most of the time, the initial concern has to do with any physical injuries for the people involved and getting help immediately. After the accident, when that initial shock has subsided, many fail to recognize how these accidents effect their emotional and mental health.
In the past few weeks, two people have contacted me seeking help for “real-Iife OCD.” I had never heard the term before, which is surprising because I am an OCD specialist. I spend roughly 75-80% of my clinical hours working with people who have OCD. I teach a course on OCD to psychiatry residents. I attend anxiety and OCD conferences every year and keep up with the latest research and treatment. So why didn’t I know about this disorder?
We all have that one feature on our face or bodies that we don’t like. Maybe your nose tip is a millimeter longer than you would prefer? Perhaps you feel that your cheekbones can be more pronounced? No matter the issue, body insecurity is common among us all. The most prominent evidence of this can be found in the media.
Death by suicide is a major public health problem that profoundly impacts families in a way few other things do. Every year, many people at risk of suicide seek and get help, potentially saving themselves and their loved ones untold grief. The good news is that death by suicide can often be prevented through early screening and obtaining effective treatment. We as a society are recognizing the critical need for these services. As awareness of this health condition increases, more and more lives will be saved.
When a baby arrives, gifts are most often given to the new little bundle of joy rather than to the new parents. Parents might find their homes heaped with adorable onesies, brightly colored chew toys, and board book editions of childhood favorites. What do new parents need? I suggest some wisdom of cognitive-behavioral therapy (CBT) from a book, a supportive friend, a group for new parents, or maybe even some sessions with a skilled therapist.
Why is CBT such a natural intervention for new moms?
Overcoming a fear of flying takes a lot of courage and practice. But it is possible with appropriate treatment. I never flew until I was almost 30 years old, and getting over my own fear of flying was one of the most difficult achievements of my life.
View the ADAA Live Webinar with ADAA members Drs. Kissen and Greene - What Are Intrusive Thoughts and How Can You Deal with Them?
If you suffer from anxiety, you probably have a contentious and complicated relationship with your mind. It feels like your mind tortures you. It gives you all these thoughts about what you should be scared of and horrible things that could happen to you.
The “unknown” is anxiety provoking for just about everyone. So how will this upcoming school year be for our teens? We don't know, and neither do they. Rightfully so, this time of year can generate lots of emotions; feelings of happiness for new school supplies, reuniting with friends and some new back to school clothes, but it can also bring up feelings of fear. The dreadful feelings associated with summer ending, the fear of new classes, new teachers and being in a new grade can all make those feelings of uncertainty and discomfort increase.
There is no doubt that coping with chronic neurological illnesses can be very distressing. What is however not frequently recognized is the fact that the distress is often a full-fledged co-morbid (co-existing) psychiatric condition that is present alongside the neurological condition. Parkinson’s Disease (PD), Multiple Sclerosis (MS), Stroke, Epilepsy and Myasthenia Gravis (MG) are some of the neurological disorders that have been identified as having psychiatric co-morbidity.
If you have made the wise decision that it is time to get help, first of all: good for you. Treatment for anxiety disorders requires a significant investment of time, energy, and effort. If you are going to invest so much, there are a few key things you can do to maximize your chances that your recovery from your anxiety disorder will be successful.
One of the more difficult symptoms of OCD that my patients deal with is the presence of mental compulsions.
Cannabidiol, or CBD, is a natural compound that has gained popularity in recent years. Here are some frequently asked questions about CBD answered by two mental health professionals who are working in this area:
1. What exactly is CBD? Is it the same as Cannabis? Hemp? Marijuana plant?
Families often ask themselves what to look for to know if their child or teen is struggling with anxiety, depression or OCD. And other families are often beating themselves up for not noticing or missing what their children are experiencing.
Discussing mental health is difficult for everyone, especially for those who experience their own mental health challenges. Our society has made this a taboo topic, which only exacerbates the issue. As we all know, when mental health is not talked about, the stigma continues, leaving people who are suffering alone and in silence. Here are some quick tips on how to stay informed for yourself and the people in your life to keep the conversation going and help end the stigma.
Educate yourself.
Living with chronic illness can sometimes feel like an insurmountable challenge. It can be demoralizing, scary, isolating, and frustrating. But there is hope. Read on to learn several helpful strategies to cope with chronic illness.
The loss of a loved one to suicide is a far too common tragedy. In 2017 alone, 47,173 people in the United States died by suicide [1] and it is estimated that an average of 135 people are exposed to each suicide death [2]. These suicide survivors include immediate and extended family members, friends, coworkers, classmates, and any others who were close to the deceased. Following a suicide loss, survivors may experience profound distress and emotional pain as well as feelings of stigma, guilt, and shame [3].
In honor of Mental Health Awareness Month, Drs. Debra Kissen and Kevin Chapman hosted a Twitter chat under the title #MythBusters where they debunked common myths surrounding anxiety and provided the actual corresponding facts.
M1: Taking some deep breaths or breathing into a brown paper bag will help you when you feel anxious.
Culture affects the way we express our thoughts, behaviors and emotions. It is therefore not surprising that there are cultural differences in the way anxiety and depression is manifested and treated. One of the main differences seen across cultures is the way anxiety and depression is expressed. Someone from a culture where it is common to know psychological terms, could easily describe anxiety and depression using those specific words. In other cultures, other words might be more common.
College is an exciting time for many young adults. It’s a time of newfound freedom, opportunity to expand one’s social network, develop new friendships, engage intellectually and consider one’s future career paths. However, it can be a challenging and stressful time for many. For many, it is the first time they are not living at home where there is a built-in support network. First time college students also have to learn to navigate a cadre of new demands, set their own schedules, find effective routines, and balance a variety of demands in order to succeed.
Imagine one morning you wake up to a loud sound of explosion, and in disbelief find out the whole city is in chaos. There is no electricity, no tap water, grocery stores are closed indefinitely, and there is no gas for the car. Control of your neighborhood constantly transitions between different groups who may treat you differently based on your religion or ethnicity, and yourself and your family are under constant threat of torture, and injuries, or even loss of life. This is what happened in Syria.
Friends and family are great at being the go-to support for the occasional ups and downs we experience in our day-to-day lives. Venting to them can feel uplifting, but in order to learn tools to overcome life’s challenges feel and feel empowered in the long run, seeking professional help may be the best route. However, sometimes there is a barrier. The most common being the costs that seems to get in between people wanting to create change but not having the funds to do so.
You can do pretty much anything you want in this life except willingly or carelessly harm others. Of all of the demands society places on us, to be hygienic, to stay healthy, to be organized and strive for protection... no burden on the self is higher than the one to do no harm, especially violent harm. So it shouldn’t come as a surprise for anyone suffering from obsessive-compulsive disorder (OCD) that this subject is such fertile ground for struggling with uncertainty.
You’re getting ready for a peaceful night sleep when you see something moving on the floor next to your bed. A spider! You yell for your braver-half to kill it. Your hero jumps into action. The shoe slams down on the hardwood. Thank goodness! Then you see the spider scurry under the bed.
“NOOO! I can’t sleep in here tonight.”
Your poor aiming hero tries to convince you that it’s a small spider who is more afraid of you. But you don’t see it that way.
“What if he crawls on me when I’m sleeping?”
Separation anxiety is something that most parents know about. Many parents will fondly recall the days when their infant could be held by anyone and then recount that there was a time with their child when this changed.
I’ve had this terrible thought I can’t get out of my head. I saw a post on Facebook from a girl I met at a party in college and remembered an incident from ten years ago. We were both pretty drunk and started fooling around. I went back to her room, and we ended up having sex. I don’t remember much else. In the morning, it was awkward, but she didn’t seem upset. We never hooked up again. I hardly ever ran into her. But when we did see each other, she was friendly. Still, I can’t stop thinking I raped her. What if I was so drunk I don’t know what really happened?
Text me when your plane lands.
Text me to let me know you got home safely.
Where are you?
How are you?
Hey did you get my last text? (sent 2 minutes ago!)
With the proliferation of cell phones, most of us have dramatically increased our checking on loved ones. In a March 2018 poll by the APA 68% of respondents said they worry about “keeping myself or my family safe.” Our cell phones are our favorite tool to keep that worry in check. But is it really working for us?
Katrina was excited. She, her sister, Maia, and their mother were on the way to the park to play handball. Suddenly, Maia screamed and collapsed on the ground, wailing. “A fly landed on me! A fly landed on me!” Her mother tried to calm Maia down, but with no success. “I’m sorry.” Katrina’s mom said, “We have to go home.” Katrina was crushed; her sister’s fears had ruined yet another family outing.
What comes to your mind when you think of Valentine’s Day? If you suffer from anxiety and worry, then there is a good chance that you are concerned about being disappointed or about disappointing someone. If you do not have a romantic partner then your anxiety might be focusing your worry on never having a partner or never finding a great love. If you are depressed, then you might be experiencing more cynical thoughts about the commercialization of the holiday, the futility of romantic relationships or your own unworthiness for a fulfilling romance.
On February 7, 2019, ADAA held a Twitter chat under the title #GotOCD. ADAA member experts Jonathan Grayson, PhD and Jenny Yip, PsyD, ABPP answered questions on the different types of OCD and treatment. Read the Q&A below:
Family members often feel frustrated and helpless as they do not know what to say or how to behave with their loved one who they may view as not being proactive in trying to get better or being irritable and negative with them.
Congratulations! You’ve graduated from college, landed your first adult job, and have moved across the country away from family and friends to enter the work force. Now what?? While these are all amazing accomplishments that highlight your transition into independence and adulthood, they also are big life changes (especially all at once) that can be very stressful.
Modern life keeps us very busy.
We find ourselves ignoring the fundamentals like our health, family, friends, community etc.
All that neglect causes dysfunction in our lives.
We try desperately to fix the problem after it becomes a significant issue. In other words, we are attempting to reverse the damage once it has already become a disorder.
As a physician, this neglect is something I see among my patients every day.
If anyone knows how stressful the holiday season can be, it’s Santa Claus. I've often wondered how he's able to keep his cool when things are heating up at the North Pole. I recently interviewed Santa and asked him how he handles holiday stress. Here's what he had to say.
KEN: Santa, how do you stay so jolly during the holiday season?
Welcome to the big leagues, kid. You’re an adult now with a new job. You’ve been working for this all your life. Don’t screw it up!
Sound familiar?
Your brain may be using different words, but if you just started a new job, there’s likely some version of it playing in your head.
October was Selective Mutism Awareness month. Even though the month is over, it’s still fresh enough on the mind to keep the conversation going, as Selective Mutism (SM) is an anxiety disorder that deserves attention. Everyone knows what anxiety is, but far fewer have heard of, or know what Selective Mutism is.
Six months ago Megan, age 32, ended her engagement. Her friends were relieved. Megan’s fiance, James, was controlling and critical. He told Megan she needed to make more money, exercise more, and come up with some interesting hobbies. Whatever Megan did wasn’t quite...enough. Megan realized that she didn’t want to marry a man like James. Megan realized how much James reminded her of her mother. Megan’s mother had always pushed her hard to excel; her disappointment left Megan devastated.
On November 13, 2018, ADAA held a Twitter chat under the title #HolidayDepression. ADAA members Mary Alvord and Shane Owens answered questions on coping with depression during the holiday season.
Q1: How common is depression during the holidays?
We conceptualize OCD as a biologically based mental health disorder whereby a person experiences intrusive unwelcome thoughts (obsessions) and engages in rituals (compulsions) to get rid of the anxiety (or any uncomfortable feeling) associated with these thoughts.
Often overlooked in conceptualizing OCD are the physical sensations that folks may focus on, rather than a primary disturbing thought.
It’s almost Halloween! My favorite holiday of the year – why? Because it’s not possible to be perfect on Halloween, and I embrace the imperfect. Other holidays have a perfect image we measure our own celebration by, but not Halloween! On this one day, the gory and the grimy rule. We all savor our shivers of fear about horrors we normally avoid. Terrifying movies! Ghosts! Devils! Spiders! All are out in force for Halloween.
People with Social Anxiety (SA) have an intense fear of being judged negatively, being criticized, or being embarrassed in public. These fears can have a profound negative affect on professional advancement. Here are examples of how two people with different types of SA fears were able to make changes that helped them achieve career success. NOTE: the identifying details of the individuals have been changed to protect their privacy.
Irritable Bowel Syndrome (IBS), an unpleasant and often debilitating condition, is characterized by frequent, recurrent abdominal pain, as well as problems with constipation and/or diarrhea. People with IBS often experience a strong urge to use the bathroom, and may avoid going to places without easy access to one. This means that many everyday locations (malls, parks, places of worship, movie theaters, classrooms, offices) feel risky, and people might start to limit their activities as a result.
Nobody likes to be criticized but it can be particularly difficult for individuals with depression and anxiety disorders. Individuals with depression tend to be highly self-critical and frequently have an ongoing internal dialogue that is harshly judgmental of themselves. Having someone else be critical can then act like salt to the wound and trigger feelings of shame at being exposed as deficient. Individuals with anxiety, particularly social anxiety, are very fearful of being judged and being criticized can feel like being under attack in a war zone!
Everyone says raising a child is easy right? Like riding a bike—once you learn how, you’ll always know how and it will never change? Wrong, oh so wrong. When it comes to raising kids, things are constantly changing. Something as small as pollen count to something bigger like sleep and diet changes, or a new school year or schedule can change everything. All of these changes come together like a perfect storm to create a child who is irrational and difficult to soothe, to change your child from the perfect kid to the exorcist—a child you don’t even recognize as your own.
On October 11, 2018, ADAA held a Twitter chat under the title #SocialAnxietyADAA. ADAA members Debra Kissen and Holly Scott answered questions on the signs and symptoms of social anxiety as well as coping tips and strategies.
1: What are the signs and symptoms of social anxiety?
Peggy, an attorney in her late 30s, establishes rituals to protect herself from aging and in her mind, becoming ugly. These rituals include 20 to 30 facial wraps a day, washing her face 40 times from morning until night, applying her cosmetics in a ritualized order, and constantly standing in front of mirrors to scrutinize the symmetry of her legs. These rituals last 8 hours a day every single day and cost over $10,000 a month to maintain.
Criticism has never been easy and people are finding that it’s getting harder to tolerate. From a young age, you quickly learn what is “trending” or “cool” and the pressure to buy into these social expectations becomes increasingly arduous for an individual to keep up with. The continuous pressure to perform at our best makes us more concerned that our chances of failing are more likely.
“Do you promise you’ll pick me up later?”
“Are you sure I’m not sick?”
“Do you promise it will be OK?”
If these questions sound familiar, your child may be engaging in excessive reassurance seeking behaviors. And unknowingly, you may be contributing to your child’s increased overall anxiety symptoms by answering those questions.
For people with anxiety, depression, or addictions, the internet can be helpful or harmful. While we can find new information, connect to resources, and use creative online coping mechanisms, the online world can be a trap and become a new place for us to engage in unhealthy, maladaptive behaviors. Medical professionals refer to these negative internet behaviors as Problematic Internet Use (PIU), but some may refer to it as internet addiction.
Ever wonder why you get “butterflies” in your stomach before doing something stressful? Or why you feel like your stomach is “tied in knots” after an argument? Ever had a meeting with a toilet that went longer than expected and it wasn’t caused by anything you ate? Stomach problems are one of the most common symptoms of stress and anxiety.
On July 11th, 2018, ADAA member experts Dr. Simon Rego @psyd and Dr. Anne Marie Albano @AnneMarieAlbano hosted a Twitter chat under the hashtag #ADAATalksSuicide, where they shared their knowledge on suicide prevention and warning signs, and how to talk to a loved one about suicide.
1. How significant is the problem of suicide in the USA? Which psychological disorders are most linked to suicide?
Rates of childhood depression have been rising in the last several years. Yet, information and awareness about childhood depression has not caught on at the same rate. Millions of people across the world wonder and doubt if children can get depressed. Many well-intentioned adults still believe that children ‘can’t get depressed. They are so young- what do they have to be depressed about? When we were that age, we were just happy’. Alongside misunderstanding is stigma and the idea that mental illness is a taboo subject.
What we now know:
It was not until my son returned from his freshman year at Emory University did he reveal what happened on our flight to Atlanta. Now back home in Los Angeles, sharing college stories with his best friend Emily, Jason disclosed to us that he was so anxious about going to Emory he threw-up in the bathroom of the plane. Emily, who spent her first year at Tulane in New Orleans, candidly offered her opinion as only a best friend can do, “You’re such a barfer. Barfing is your go-to when you’re anxious.” I asked Emily, what was her go-to? “Oh I’m a crier.
The recent suicides of Kate Spade and Anthony Bourdain has placed the spot light on the growing problem of suicide. It has triggered conversations on the topic and caused many people to question why such successful and seemingly happy people who had everything going for them would take their own lives. Suicide is a heart-breaking problem that is growing and needs to be addressed in as many ways as is possible. Understanding the risk factors, knowing the warning signs and what to do about them, is a crucial step. The more the awareness the greater the impact on suicide prevention.
In a recent article, USA Today explored the growing field of apps targeted towards mental health and mental health treatments. The article claimed that millions of Americans are turning to apps to provide therapy treatments and explored the usefulness of such resources for improving mental health.
The current border crisis where children are being forcibly separated from their parents has many of us wondering about the impact of such a practice. As a child psychologist who understands the effects of trauma on a child’s mental health, cognitive and emotional development, physical health, social adjustment, interpersonal formation, and academic challenges, I am disheartened by what these innocent children have been experiencing. As a mother, I am filled with anguish when imagining the utter fear and terror of a child being pulled away from the safety of a parent or loved one.
As a clinical psychologist, I probably think about suicide more often and in different ways than most. I’ve read the research. I’ve been trained to ask the hard questions. I am all too familiar with the frustrating gaps in our knowledge base: what causes it, who is at risk, how do we prevent it? I understand the stigma and misconceptions surrounding it, and I know, firsthand, the collateral damage that stems from it.
Updated October 2020
What You Need to Know About Treatment and Medication Options
Many of you, like me, follow a number of news sources throughout the day. Whether radio, television, e-news sites, or newspapers, there are a myriad of ways that people can easily access information 24/7. This proliferation of information is wonderful – but it can be overwhelming and in some cases – especially around mental health issues – inaccurate or simply untrue.
In honor of Mental Health Month, the Anxiety and Depression Association of America held a Twitter Chat under the title #GotPanic? ADAA members Dr. Debra Kissen @LightOnAnxiety, and Dr. Kevin Chapman @drkchap answered Twitter's questions around symptoms, management & the treatment of panic disorder.
With the deluge of information on this event, it is highly likely that your children, preteens, and teens have heard a lot about the event and may have even seen some of the video coverage of the shooting itself and the aftermath. The key message for parents to convey after exposure to any type of trauma or violence is to ensure that your child feels safe and loved.
La ansiedad es una emoción natural que nos ayuda a dirigir nuestra atención hacia posibles amenazas. Aunque necesitamos la ansiedad para sobrevivir, en ocasiones se puede convertir en un problema. En particular, si la ansiedad ocurre sin ninguna razón, es una reacción exagerada al estresor o nos crea disfunción en nuestras vidas podría ser señal de un trastorno de ansiedad.
Anxiety is a natural emotion that directs our attention to possible threats. Although we certainly need anxiety to survive, it sometimes can be a burden. This is especially true when anxiety appears without an identifiable stressor, is out of proportion to the stressor or creates dysfunction in our social or professional lives. If the anxiety presents with any of these characteristics, then it might be part of an anxiety disorder, such as Generalized Anxiety Disorder, Social Anxiety Disorder, Panic Disorder, Specific Phobia or Post-Traumatic Stress Disorder.
Worryland: Familiar Territory for Women with Narcissistic Parents: Caroline’s diamond solitaire glitters on her clenched left hand. She’s engaged to Ryan, a man she truly loves. However, Caroline’s happiness comes with a warning: her mother, Trudy. Already Trudy has told Caroline that if she invites her future mother-in-law to go wedding dress shopping with them, then Trudy is not coming. She’s the mother, and it’s her day. Worry keeps Caroline awake at night. Maybe she and Ryan should just elope.
Unwanted intrusive thoughts are stuck thoughts that cause great distress. They seem to come from out of nowhere, arrive with a whoosh, and cause a great deal of anxiety. The content of unwanted intrusive thoughts often focuses on sexual or violent or socially unacceptable images. People who experience unwanted intrusive thoughts are afraid that they might commit the acts they picture in their mind. They also fear that the thoughts mean something terrible about them.
Anxiety disorders are the most common mental health disorder in the United States. Data show that for Black women, anxiety is more chronic and the symptoms more intense than their White counterparts. This description, however, only tells half the story. What it does not tell us is how anxiety is perceived and experienced daily by Black women.
The Autism and Obsessive Compulsive Spectrum Program and the Anxiety and Depression Program at the Albert Einstein College of Medicine and Montefiore Medical Center :
https://www.einstein.yu.edu/departments/psychiatry-behavioral-sciences/autism-program/
Spectrum Neuroscience and Treatment Institute:
http://www.spectrumneuroscience.com/
Intimate partner violence (IPV) takes place in all settings, in all socioeconomic, religious, ethnic, and cultural groups. The overwhelming global burden of IPV is endured by women, and the most common perpetrators of violence against women are male intimate partners or ex-partners. However, women who are experiencing IPV often do not see themselves as abused.
People who identify as sexual (i.e., lesbian, gay, bisexual, queer) or gender (i.e., transgender, genderqueer, non-binary) minorities have similar symptoms of anxiety and depression as heterosexual and cisgender (non-transgender) individuals. Although the symptom presentation may be similar, sexual and gender minority individuals generally experience additional identity-based stressors that can contribute to the development of anxiety and depression, and that are relevant to their treatment.
An underappreciated tool for successful living is “The Art of Disengagement.” There is much literature around engagement and holding one’s ground, but disengagement often gets the short end of the stick.
It takes much skill, mental training and control to disengage. When your brain is sending you a signal “this is very critical to survival” it becomes hard to then note this as a false alarm. Choosing to attend to a different stimuli can feel like it requires a black belt in mental training.
Holidays often come with the pressure to entertain and be a “perfect” host. Being perfectionistic in the details of holiday planning, can ruin the fun for ourselves, as well as those around us. While most people are happy to be around friends or family, enjoying good food, drinks and the sight of kids opening gifts, for certain people, the thought of something being out of place, someone not getting their favorite dish or the decorations falling short, can cause significant feelings of distress. People who struggle with anxiety disorders, such as social anxiety or panic di
Often patients, in the course of their treatment for OCD, will question whether they actually have OCD or not. This doubt feels different to them than the doubt arising from the intrusive thoughts that initially brought them into treatment. But this doubt about having OCD is OCD! OCD demands certainty and convinces the sufferer that bad things will happen if they’re not certain. The content of the intrusive thoughts is always irrelevant, but the content can distract patients (and sometimes clinicians) from dealing with uncertainty and risk.
There is no right way to handle trauma. Each individual moves at their own speed and has their own readiness to confront pain and suffering.
So, you’re a failure. Fine. Get on with your life! In my work as a psychologist treating anxiety disorders, I’ve learned that often an underlying driving fear in my patients is the worry that they are failures. (My patients and I use a more colorful term, but for editorial purposes I’ve changed the phrase.) They have intrusive thoughts that they have or will mess things up in some way and cause harm to themselves or others.
Reviewed October 2020
The biggest fear of individuals with Social Anxiety Disorder (SAD) is that of being found to be deficient and judged for the deficiency.
Since 1949, May has been known as Mental Health Awareness Month. Each year, when May is over, I wonder why we’re not encouraged to be aware of our mental health all year, every year, just as we are for our so-called physical health.
General guidelines for youth mental health: Teach them compassion and gratitude
Teaching children how to be compassionate towards others inspires this behavior towards themselves. Encourage your child to be kind and caring to others by modeling unconditional acceptance. Acknowledge and admit your own mistakes in front of your kid. When they go through rough times, teach them to take the time to take care of themselves to re-energize.
In my first meeting with new patients who struggle with OCD and anxiety, I explain that the type of psychotherapy I practice, Exposure and Response Prevention, involves encouraging them to feel uncomfortable. It’s a type of therapy that they will not particularly “enjoy,” but it’s a therapy that will hopefully get them back to enjoying their lives.
Reviewed October 2020
Everyone has bad days when things just aren’t going well and we just feel off. This can be in response to some bad news like getting a grade that is less than stellar or your friends are too busy to hang out. Sometimes when we find our bad day seems to last day after day, then that may mean something else is going on.
Updated October 2020
The decision to take medication for mental health is a very important one, and it often takes place when symptoms of anxiety, depression, or other mental health issues have intensified, which can make the decision process much harder. The following questions can help ease the process and guide you in your conversation with your doctor and in the ongoing treatment process.
Ask Your Doctor:
Many people wonder if their therapy is really helping them overcome their problem. Why? They often have therapists who tell them that they are doing well, but their therapist does not make clear to them what they mean by making progress. Does it mean facing your emotions, being able to talk about difficult things, or does it mean that you feel better and function better? Many people also like their therapist’s kindness and empathy, but feel guilty about questioning the outcome because their therapist is so nice even though they are not getting better.
It’s easy to understand how a major car accident would cause someone to fear driving, but most driving phobia have nothing to do with accidents.
Here is a list of the top 5 driving fears:
Everyone’s skin crawls when they hear nails on a chalkboard (remember chalkboards?). But if your body reacts with extreme discomfort at the sound of everyday noises, like chewing, slurping coughing and tapping, you might be suffering from Misophonia, literally translated as “the hatred of sounds.” Although not recognized as a genuine disorder, the symptoms are genuine for those who suffer. Negative emotions, thoughts and physical reactions are triggered by specific sounds and they can be overwhelming.
One of the key issues that consumers ask us about is how to identify warning signs in adolescents regarding anxiety and how to raise the issue with their adolescents.
Children of anxious parents are more at risk for developing anxiety disorders. This is because they will have both a genetic predisposition to developing an anxiety disorder and their environment may emphasize hyper vigilance to risk cues. It is important to emphasize that being at risk for developing an anxiety disorder does not mean with certainty that they will develop one. Creating an emotionally healthy environment where children learn to tackle their fears can prevent the development of an anxiety disorder.
Social Media outlets like Facebook, Snapchat, and Instagram have become a behemoth daily presence in our lives. Facebook COO Sheryl Sandberg recently reported there are an astonishing 1.23 billion daily log-ons to the social media giant per day, representing an 18% increase in the last year (as of September, 2016). CEO Evan Spiegel’s app Snapchat offers users an experience where video, photo and text messages are live for only 24 hours- allowing for an instant and fleeting connection between people.
Step 1: See Through OCD’s Scare Tactics
Whether my patients have OCD, social anxiety, a phobia, panic, or are just generally anxious about life, they come into treatment wanting to be free of the uncomfortable feelings associated with anxiety. To rid themselves of their anxiety they have tried meditation, relaxation, yoga, different psychotherapies and medication, but overall they don’t feel a whole lot better. They ask me, “Why am I so anxious?” and “How do I get rid of this anxiety?” And I respond: “You need to allow yourself to be anxious and you don’t need to know why you are anxious.” I know it sounds counterintuitive.
Many Americans are experiencing a higher level of worrying since the presidential election. Our country is in midst of a big transition and the stakes are high. We don’t know what will happen and uncertainty is worrisome for many.
As an anxiety disorder therapist, I’ve worked with many people who worry. Can I apply what works with chronic worriers to political anxiety?
Suicide is one of the most devastating public health problems faced by society today. In the United States, suicide is the 10th leading cause of death (Centers for Disease Control and Prevention [CDC], 2015). Over 44,000 Americans take their own lives each year, which works out to about 120 suicides each day, just in the U.S. (CDC, 2015). This means that we are each more likely to die by our own hand than someone else’s (World Health Organization [WHO], 2012).
As my OCD patients get better with treatment, they are relieved that their obsessions are less frequent and less intense and they have more control over performing rituals. This they expect. But what can be unexpected is the feeling of mourning as symptoms dissipate. Often my patients have lived most of their lives struggling with upsetting obsessions and engaging in rituals that can consume hours of time. Their lives have been severely compromised by the disorder. They certainly don’t like having OCD, but it’s familiar to them.
Naturally, when individuals seek treatment for anxiety, their primary goal is to “stop…worrying/panicking/obsessing/etc.” This is understandable because the symptoms have caused turmoil in their lives!
Many of my patients took an extended holiday over the Christmas/New Year's break. When they returned to treatment in midJanuary most of them reported that their OCD symptoms had worsened. Obsessions returned that had been dormant. New obsessions and compulsions emerged and sometimes they didn’t realize this was OCD because the content of the OCD was unfamiliar. Compulsions they had been successful resisting in the past were much harder to resist. If you have OCD, it’s helpful to understand what may happen when you go on vacation.
We are in the home stretch of a prolonged, caustic, and shocking presidential campaign season. No matter which way you lean, few will argue that the 2016 election will go down in history as unprecedented, in that both candidates seem have a surplus of skeletons in their closets and a penchant for throwing surprise curveballs.
1. Latch on to triggers that set you off.
Figure out what frightens you and examine how your anxiety reaction is triggered. Your goal is to identify your particular triggers, so you can manage your fear when anxiety levels are low. Learning what sets you off makes it easier to turn it off.
The fear of vomiting can become so all-consuming and terrifying that eating becomes a struggle and weight loss becomes dangerous. As sufferers try to protect themselves from throwing up, their world shrinks until it becomes impossible to work, go to school, or to socialize. This was Kay prior to treatment. In this live free webinar, Ken Goodman, author of The Emetophobia Manual, interviews Kay, one of his former patients. Together they discuss her remarkable healing journey and how she freed herself from the fear of vomit and reclaimed her life.
More than 40 million adults in the United States suffer from some form of anxiety. Sadly, only one-third recognize what may be happening and talk to their doctor; only about one-quarter of African Americans seek mental health care, compared to 40 percent of whites.
College is typically a challenging experience with some expected highs and lows. For some it is also the time during which common mental health problems start. Because of this, you have to talk to your kid about mental health before school starts.
This conversation must include these topics:
“Oh, the places you’ll go!” exclaimed Dr. Seuss, as he he hoped to inspire children to live a vigorous life of travel, exploration, and discovery. But for people with severe anxiety, travel could be considered the ultimate discomfort zone. A variety of unknowns can cause a cyclone of negative thoughts: “How will I get there? Will I be able to adjust to an unfamiliar environment? How do I deal with anxiety while I’m away from home?”
I recently discovered that two friends of mine suffer from trichotillomania, or compulsive hairpulling. It came as a surprise to me, and even as a clinical psychologist, it was difficult to detect because neither one of them pulls out their hair in an obvious manner. Although about 3 percent of the U.S. population experiences trichotillomania during their lifetime, few people know what it is — and even fewer want to talk about it, which adds to the elusiveness of this disorder.
Reviewed October 2020
In the early years of my career as a clinical psychologist and psychotherapist I often struggled to find a way to help some of my clients cope with their thoughts and feelings of regret: “If only I had recognized my cheating boyfriend for what he really is,” or “I wish I’d been a better and more patient mother to my son,” and “If only I’d studied harder I would have done better in life.”
Updated October 2020
If you’re lesbian, gay, bisexual, transgender, or queer(LGBTQ) or are exploring your sexual orientation or gender identity, and you struggle with anxiety or depression, let’s start by putting things into context. By that I mean let’s think through powerful life experiences that fundamentally impact your sense of well-being.
Anxiety and Depression for Lesbians, Gay Men, Bisexuals, and Transgender People
It happens on a daily basis. I routinely scroll through my Facebook feed while sipping my morning tea. That's when I see photos and status updates about people doing things: going to fabulous charity events, attending basketball games from the company box, brunching at the newest hotspot, or sipping mojitos on an exotic beach, and all with perfectly filtered photographic evidence to show for it. Thanks to the wonders of 4G, these friends’ day-to-day lives have somehow become part of my own too.